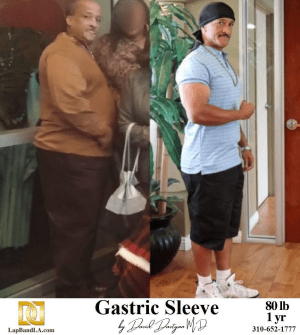
Surgical interventions for weight management, such as the gastric sleeve, have increased considerably over the past decade, reflecting the growing prevalence of obesity and the search for more effective treatments. With an increasing number of patients seeking permanent solutions to weight-related conditions, it becomes imperative to provide comprehensive knowledge not only about the procedure itself but also the long-term nuances of living with a gastric sleeve. This post explores the requirements for gastric sleeve surgery, its risks and reversibility, and elucidates aspects rarely disclosed during pre-surgical consultations.
Readers will acquire a factual understanding of the gastric sleeve, drawing upon peer-reviewed clinical evidence and real patient outcomes. The intended audience includes individuals considering bariatric surgery, patients currently navigating the complexities of postoperative adaptation, and healthcare professionals seeking a more nuanced perspective on patient education.
A Precise Overview of Gastric Sleeve Surgery
Defining the Gastric Sleeve Procedure
The gastric sleeve, or sleeve gastrectomy, constitutes a restrictive bariatric procedure wherein a significant portion (roughly 80%) of the stomach is excised, leaving a slender, tube-like structure. This alteration reduces gastric capacity, thereby promoting early satiety and significant weight loss. It is remarkable for its permanence; unlike adjustable gastric bands, the excised portion of the stomach cannot be replaced, and thus the anatomical change is irrevocable in most cases.
Indications and Requirements for Gastric Sleeve Surgery
Criteria for patient selection are stringent. Typical requirements for gastric sleeve candidates include:
- A body mass index (BMI) ≥ 40, or ≥ 35 with serious obesity-related comorbidities (such as type 2 diabetes, hypertension, or obstructive sleep apnea)
- Demonstrated failure of conservative medical and lifestyle interventions
- Comprehensive understanding of postoperative dietary, behavioral, and lifelong nutritional commitments
- Psychological readiness and stable mental health status, as determined by psychological evaluation
Eligibility is further nuanced by consideration of age, prior surgical history, and specific comorbidities that could contraindicate surgery.
Gastric Sleeve Risks and Considerations
No surgical procedure is without inherent risks. The gastric sleeve entails the possibility of perioperative as well as long-term adverse outcomes. These may include:
- Surgical Complications: Hemorrhage, infection, and staple line leakage, the latter carrying grave consequences if undetected
- Nutritional Deficits: The removal of the gastric fundus, a site critical for absorption of certain nutrients and for the production of intrinsic factor, predisposes to deficiencies in vitamin B12, iron, calcium, and folate
- Gastroesophageal Reflux Disease (GERD): Paradoxically, some patients report exacerbation or de novo development of GERD postoperatively
- Weight Regain: Although initial weight loss is often significant, epidemiological data suggests that a subset of patients may experience partial weight regain, particularly if postoperative lifestyle recommendations are not strictly observed
What They Don’t Tell You About the Gastric Sleeve
The Profound Psychological Shifts
It would be reductive to characterize the gastric sleeve solely as an anatomical adjustment; it is no less a catalyst for psychological transformation. Postoperative euphoria resulting from rapid weight loss is not universal; many individuals must confront enduring patterns of emotional eating, body image dysmorphia, or shifting dynamics in social and familial relationships. The implication is clear: long-term psychological support must feature as centrally as nutritional counseling in any post-bariatric care protocol.
Social and Behavioral Adaptations
Contrary to common assumptions, the requirements for gastric sleeve surgery persist long after the operating room. Patients are obliged to:
- Adapt to Distinct Eating Habits: Meals are restricted to minuscule portions, necessitating mindfulness and prolonged mastication to avoid gastrointestinal discomfort.
- Eschew Certain Foods and Drinks: Carbonated beverages, fibrous or tough meats, and foods high in added sugar and fat can provoke dumping, nausea, or vomiting.
- Commit to Life-Long Supplementation: Given the certainty of micronutrient deficiencies, daily vitamin and mineral supplementation remains essential.
Not infrequently, social events and holidays become fraught with anxieties over dietary slip-ups or being perceived as “high maintenance” by peers, underscoring the social adaptability required for long-term success.
Schedule a Consultation!
Is Gastric Sleeve Reversible?
This is a crucial matter, often subject to misconception. Unlike procedures such as the gastric band, the sleeve gastrectomy is not reversible; the excised stomach tissue cannot be restored. While gastric bypass “revisions” are sometimes possible, the vast majority of sleeve patients must regard the surgery as permanent. Secondary or “conversion” operations, such as conversion to a gastric bypass in cases of severe reflux or inadequate weight loss, are considered major surgeries that carry their own risks.
Practical Nuances of Life After a Gastric Sleeve
Short-Term Postoperative Course
The immediate period following surgery is characterized by a staged dietary progression—from clear liquids to pureed foods, advancing to regular, albeit restricted, meals over several weeks. Close clinical monitoring is indicated to detect early complications and to adjust supplementation regimens.
Long-Term Adaptations
Nutritional Management
The reduction in stomach volume necessitates disciplined adherence to high-protein, low-carbohydrate meals, fractionated into five or six small portions daily. Lifelong avoidance of high-glycemic foods is recommended to mitigate reactive hypoglycemia and excessive weight regain.
Physical Activity and Monitoring
Sustained weight loss and metabolic benefit are inextricably linked to graduated increases in physical activity. Periodic laboratory and clinical evaluations are essential for timely identification and correction of nutritional deficiencies.
Coping with “What They Don’t Tell You”
Many patients report feeling unprepared for the extent of lifestyle adaptation. There is woefully little literature on the subtle challenges, such as hair loss, altered medication absorption, altered alcohol metabolism, or unanticipated psychological burden, all of which may profoundly impact quality of life.
Addressing Frequently Asked Questions
What Are the Absolute Requirements for Gastric Sleeve Surgery?
Patients must meet BMI thresholds, have documentation of failed non-surgical attempts, pass psychological assessment, and demonstrate readiness for lifelong dietary and behavioral modifications.
What Risks Should Be Weighed Most Heavily?
While the early risks of staple line leak and hemorrhage are significant, the more insidious risks center on micronutrient deficiencies, exacerbation of GERD, and possible psychological distress.
Is the Procedure Reversible?
No, the gastric sleeve is considered permanent. Only under rare, complex circumstances is conversion to an alternative bariatric approach considered.
Taking an Educated Step Toward Gastric Sleeve Surgery
The decision to undergo a gastric sleeve is momentous, characterized by permanent anatomical and psychosocial changes. While the weight loss outcomes can be compelling, prospective patients must approach the process with a sophisticated grasp of both surgical facts and lived realities. At Davtyan Medical Weight Loss and Wellness, we prioritize a multidisciplinary approach, ensuring preoperative education and longitudinal support to optimize both physical and psychological outcomes.
Visit Dr. Davtyan at our Weight Loss Clinic in Los Angeles and experience the care of a true expert in the field of weight loss surgery. At Davtyan Medical Weight Loss and Wellness, Dr. David G. Davtyan leads with compassion, professionalism, and unmatched expertise. With prestigious board certifications in Surgery and Bariatric Medicine, Dr. Davtyan is a respected figure in the Los Angeles weight loss community. His personal experience with weight loss gives him unique empathy and a deep understanding of his patients’ journeys, transforming their challenges into empowering steps toward health and wellness. Dr. Davtyan is not only a highly skilled weight loss surgeon but also an experienced oncologist, bringing a comprehensive, patient-centric approach to bariatric care. He prioritizes long-term health over quick fixes, guiding patients to adopt sustainable lifestyle changes that support lasting success. At Davtyan Medical Weight Loss and Wellness, patients are more than just numbers—they are partners in a mission to achieve better health and a brighter future. Visit Dr. Davtyan today and take the first step toward your own life-changing transformation.Visit Dr. Davtyan in Los Angeles